What is Biofilm?
Acute infections caused by pathogenic bacteria have been studied extensively for well over 100 years.
These infections killed millions of people in previous centuries but have been combated effectively by the development of modern vaccines, antibiotics and infection control measures.
Most research into bacterial pathogenesis has focused on acute infections, but these diseases have now been supplemented by a new category of chronic infections caused by bacteria growing in slime-enclosed aggregates, known as biofilms.
Biofilm infections – such as pneumonia in cystic fibrosis patients, chronic wounds, chronic otitis media, & implant or catheter-associated infections – affect millions of people worldwide each year, resulting in many deaths.
Bacteria have two life forms during growth and proliferation – unicellular and multicellular. Unicellular life forms, known as planktonic bacteria exist as free-living bacteria. Whereas multicellular life forms live in a self-produced matrix that allows them to attach to inert or organic surfaces. This latter form is commonly referred to as the biofilm growth phenotype.
Acute infections are generally treatable with antibiotics and are assumed to involve planktonic bacteria.
However in cases where the bacteria succeed in forming a biofilm within the human host, the infection often turns out to be untreatable and can develop into a chronic state. This is because biofilms allow cells to live in a coordinated, more permanent manner that favor their proliferation.
The Hallmarks
of Chronic Biofilm-Based Infections
- Extreme Resistance to Antibiotics & Many Other Conventional Antimicrobial Agents
- Extreme Capacity for Evading the Host Defenses
What are Bacterial Biofilms?
Biofilm formation is considered to be the way microbes adapt to hostile environments.
Bacterial biofilm is widely found in natural environments with water, and also in human diseases, especially in patients with indwelling devices for the purpose of medical treatments. With the progress of medical sciences, more and more medical devices and/or artificial organs are applied in the treatment of human diseases; increasing the number of surfaces that are at risk of biofilm formation.
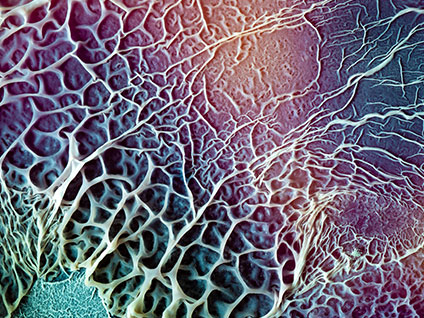
Biofilm is a structured consortium attached on a living or inert surface formed by microbial cells. These cells are adhered to each other and are surrounded by the self-produced extracellular polymeric matrix, known as biofilm.
The Typical Development
of Biofilm Includes Several Stages
- Attachment to a Surface
- Formation of micro-colonies
- Development of young biofilm
- Differentiation of Structured Mature Biofilm
- Dispersal of Mature Biofilm
